Hip Replacement
Anterior Hip Replacement
Anterior hip replacement is a muscle preserving surgery with recognized outcomes and high success rate
Anterior hip replacement is a muscle preserving surgery with recognized outcomes and high success rate
The procedure eliminates hip pain by resecting the degenerative parts and replacing them with artificial parts.
For those looking to schedule Hip replacement surgery for themselves, the website https://www.orthopaedicsurgery.ie will explain every aspect of the procedure. Starting from prior preparation to rehabilitation and long-term care, many factors influence the benefit you get from your newly replaced hip.
The members of our Orthopaedic team will walk you through the entire process using interactive demonstrations and videos. This way, you can learn valuable tips and tricks to ensure a speedy recovery and long-term benefit.
Pre Assessment Clinic
Hip replacement recommendations mainly depend on the extent of the patient's pain and disability. Therefore, before recommending the process, the orthopaedic surgeon, Dr. Merghani, will conduct a complete individual evaluation of each patient.
This process is held in the clinic, where the doctor looks at your medical history. After that, he will assess your physical aspects, such as the strength, alignment, and mobility of your hip bone.
Finally, additional X-rays will confirm the exact deformity or damage inflicted on your hip bone if a problem is detected. Besides that, MRI scans may also be recommended to get a complete picture of the bone and soft tissues in the area.
Once the need for hip replacement surgery is confirmed, the Pre Assessment team reviews whether you are fit enough to go through the surgery. Mainly, this involves several investigations and blood tests to suit your health.
Additionally, you will be recommended medications to improve your health before surgery if needed.
After that, you can discuss the implant options available for you with your orthopaedic surgeon, Dr. Merghani. He will map out the suitable option for you depending on your health, age, and weight.
Also, he will clarify any questions you have regarding the procedure during your outpatient visits before your surgery.
Why Would You Need Hip Replacement Surgery?
Arthritis or damage to the articular cartilage is the most common cause leading to hip replacement surgery. Now, whether you need surgery entirely depends on the extent of damage inflicted upon the articular cartilage.
Usually, arthritis is diagnosed upon groin pain and knee pain. While doctors initially prescribe pain relief medication and physiotherapy to treat arthritis, hip replacement surgery is recommended when all other methods have been exhausted.
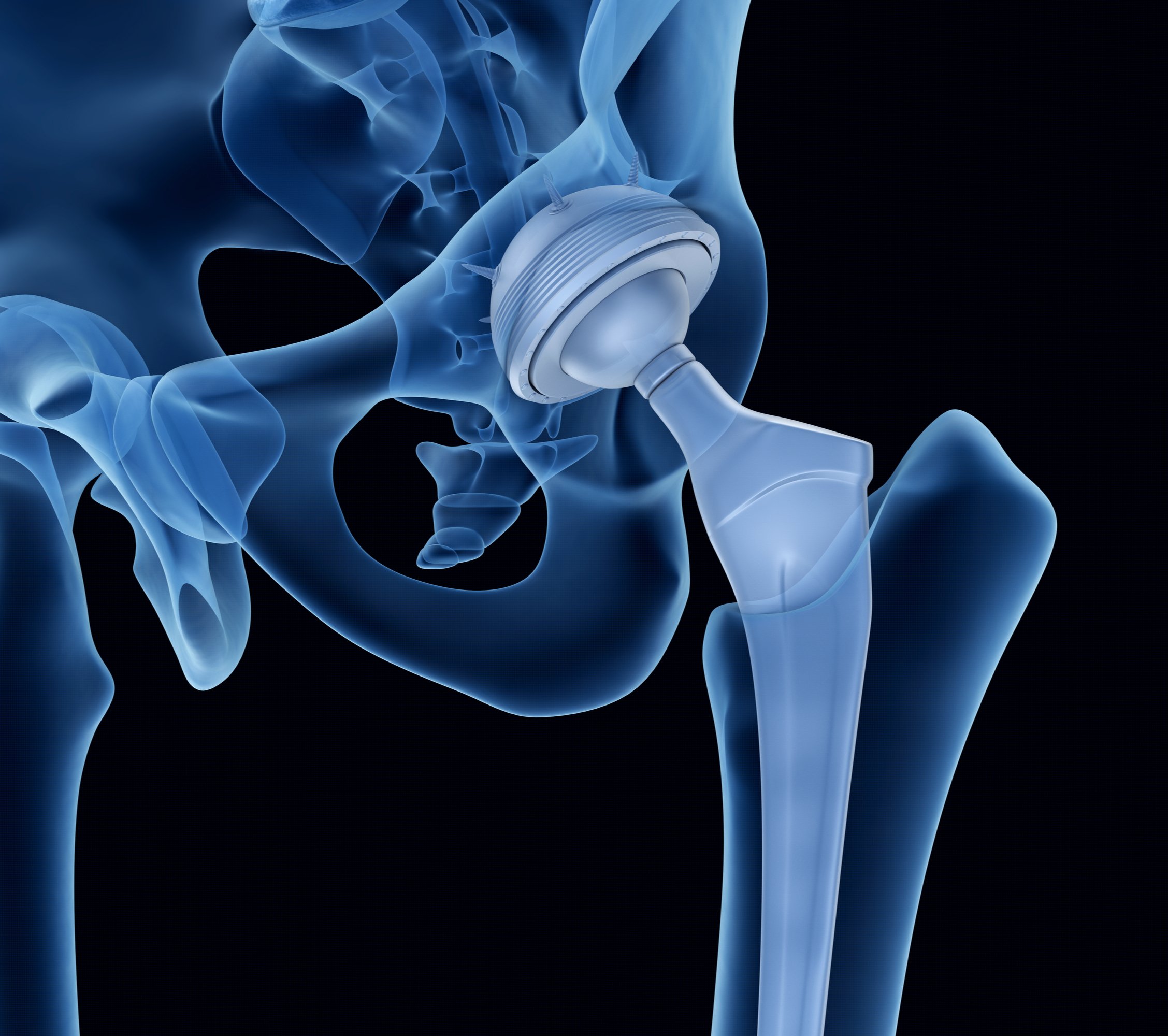
What are Hip Replacement Prosthetics Made up of?
Based on your physical health and the extent of your injury, you will be recommended a hip replacement that works best for you. Usually, these prosthetics are made of titanium alloys or other metals with polyethene or ceramic coating.
Furthermore, different materials are used to fix the socket in its place. This material also varies from a special bone cement or a coating that encourages bone growth over the implants.
Apart from the material, fixing the hip replacement also varies for each case and patient. These factors will determine your recovery time and the location of your case. All these facts will be explained to you by your surgeon, Dr. Merghani.
Complications of Hip Replacement Surgery
- Frequent (10%)
- Common (2-5%)
- Infrequent (1-2%)
- Rare (<1%)
- Urinary Tract Infections
Can occur frequently following surgery. It is important to drink loads of water following surgery to try to prevent this. If you notice any buring or stinging tell your healthcare team.
- Blood Clots - Deep Vein Thrombosis
- Bleeding
- Nerve Injury
- Dislocation
- Leg Length Discrepency
- Difficulty passing urine
- Loosening of the hip
Mobilising following surgery by taking frequent walks, staying well hydrated and anti clotting medications will help prevent blood clots.
During surgery you can bleed. Medication is sometimes used to reduce this. If bleeding is significant you may require a blood transfusion. If you have religious beliefs with regard to blood transfusion you must inform your surgeon.
The siatic nerve which runs down the back of your leg can get streched during the procedure. If this happens it can cause a foot drop which can be permanent or temporary and involves wearing a foot splint to help control your foot.
This happens when the ball of the hip comes out from its socket. Strict adherence to the hip precautions will reduce tyhe chance of this happening.
Surgery will aim to ensure your legs are equal lengths. Sometimes this is not possible and there may be a difference in the length of your legs. It can also be an issue if you have arthritis in the other hip.
5% of patients require a urinary catheter for the 24 hours following surgery. It is most common in patients who have a history of difficulty passing urine eg prostate conditions
Over time eg 10-20 years the hip can loosen. If this occurs it may be necessary to have further surgery to replace your hip replacement.
- Superficial Infection (cellulitis) is an infection of the overlying skin. This occurs in the weeks following surgery and can be treated with antibiotics. If you notice any redness around your wound contact your orthopaedic team immediately.
- Deep Joint Infection - Early & Late
Infection
There are different types of infection that can occur following a hip replacement which occur at different times up to years later.
There is a higher risk associated with smoking, obesity, diabetes and immunocompramised patients. Many strategies are used to try to prevent this occuring such as antisceptic washes, sterilistaion techniques, antibiotic use etc
2 in every 1000 patients die within one month of surgery. Risk is increased for patients with medical comorbidities such as heart or lung problems.
This is one of the most worring complications as the impact on the patient is so significant.
It may be necessary to washout the joint, remove the hip replacement and put in a spacer (a temorary hip with antibiotics) and when the infection has cleared up, put in a new hip replacement.
Patients require prolonged courses of antibiotics for several months.
- Death
- Nerve Damage
- Fracture
- Pulmonary Embolus
2 in every 1000 patients die within one month of surgery. Risk is increased for patients with medical comorbidities such as heart or lung problems.
0.1-0.2% (1-2 patients per 1000) of patients will have damage to the femoral nerve or obturator nerve in the groin and this can cause chronic pain in the groin region.
Rarely the femur or acetabulum can fracture when the implants are inserted. This can result in the need for further surgeries (a revision hip replacement)
A clot forming in the lungs is a rare complication and can result in a wide severity of symptoms from mild cough to death.
Post Operative Care
- Hospital Care
- Rehabilitation
- Long Term Care
1-5 Days
A patient will need to stay around 1-5 days at the hospital after the procedure to ensure a smooth transition. The orthopaedic team will help the patient develop a healthy diet plan while keeping their blood sugar under control during this time.
While most patients do well medically after the procedure, the main focus remains on developing a proper rehabilitation plan for fast recovery.
0-6 Months
Upon being discharged from the hospital, patients have to follow an exercise program prescribed by a physiotherapist at home. This therapy helps them regain their muscle strength for everyday activities.
You will have to carry out these exercises at least six months after the procedure. Besides that, follow-up examinations include a wound checkup at two weeks, followed by an additional x-ray at six weeks.
Finally, you can continue your daily activities after a complete checkup six months post-operation.
1-5 Years
After the rehabilitation period, patients will have checkups to assess their condition at two and five years. If you have any concerns regarding your progress, they will be addressed during these sessions.


